One out of three people has had problems sleeping in their lifetime. But there is a big difference between having trouble sleeping from time to time and having a serious, chronic sleep disorder.
Sleep disorders are common among Americans and can affect every part of their lives. They can limit productivity, concentration, and ability to maintain relationships. Sleep disorders are also harmful to physical and mental health, and they’re especially common among Veterans. If you are a Veteran struggling with sleep, you are not alone: Did you know that up to 50% of Veterans enrolling in VA health care have Insomnia Disorder? The two most common sleep disorders, Insomnia Disorder and Obstructive Sleep Apnea, are widespread among Veterans.
There are many reasons why Veterans are more likely to develop sleep disorders than the general population. During military service, many Veterans are in stressful and difficult work situations. It is common to work irregular hours or have to stay awake for long periods of time to be alert to the dangers of combat. This can lead to Insomnia Disorder. Symptoms of Insomnia Disorder include having trouble falling asleep, staying asleep, or waking earlier than you want to on a regular basis. It’s also associated with medical conditions such as cardiovascular disease, obesity, and diabetes. Insomnia can make you feel less than your best during the day, and cause you to feel anxious, depressed, or irritable.
Usually, insomnia symptoms are first brought on because of stressful life events, such as military training, deployment, trauma, emotional distress, or illness. During that stressful period, it is normal for your habits to change to cope with not getting enough sleep. Even thoughts and beliefs about sleep can change. But after the stressful period ends, the problems with sleep can remain due to the coping strategies used that were actually unhelpful. Ironically, these unhelpful strategies turn into the cause of the ongoing insomnia.
It’s common for Veterans to experience both insomnia and ongoing irregular sleep patterns well beyond military service. After years of poor sleep, your body and mind may need to relearn how to sleep well again. This often requires help.
Another sleep problem many Veterans face is Obstructive Sleep Apnea. Obstructive Sleep Apnea is a sleep condition involving a block in the airway during sleep, causing breathing to stop. It is a serious health condition that can increase the risk for high blood pressure, heart disease, stroke, diabetes, and depression. One of the main symptoms of sleep apnea is loud snoring. Since people often don’t know that they snore during sleep, many people with sleep apnea don’t know that they have it. In fact, many people only talk to their doctors about their symptoms because someone close to them, such as a spouse or child, sees them having trouble breathing while they sleep. Identifying sleep apnea symptoms and diagnosing this condition is the first step in helping treat Obstructive Sleep Apnea.
Although Insomnia Disorder and Obstructive Sleep Apnea are the two most common sleep disorders, there are many others that often go undiagnosed. Few doctors are trained to recognize the symptoms of these less common sleep disorders. Yet, left untreated, any sleep disorder can negatively impact health and quality of life.
To help Veterans understand their sleep problems and receive effective treatment, VA sleep experts created a Sleep Check-up tool. Sleep Check-up includes a five-minute questionnaire with customized questions that help screen for the sleep disorders you may be experiencing. It also includes videos of Veterans sharing their experiences with sleep disorders and downloadable fact sheets about sleep disorders that you can print out and share with your provider.
If you think your poor sleep quality is caused by a sleep disorder, use VA’s Sleep Check-up and take a self-screening.
Be sure to check back soon for the second blog in our series, which will focus on how to manage insomnia symptoms.
This blog post is the first in a series about understanding sleep disorders and options for treatment.
Christi Ulmer, PhD, DBSM, and Carolyn Greene, Ph.D., work at the Durham VA Medical Center
Topics in this story
More Stories
Health summit gave Veterans opportunities to visit with VA staff and meet community organizations that provide services to Veterans.
STAR is a rehabilitation program for Special Operations Forces service members and Veterans. It facilitates recovery, function, reintegration, and transition.
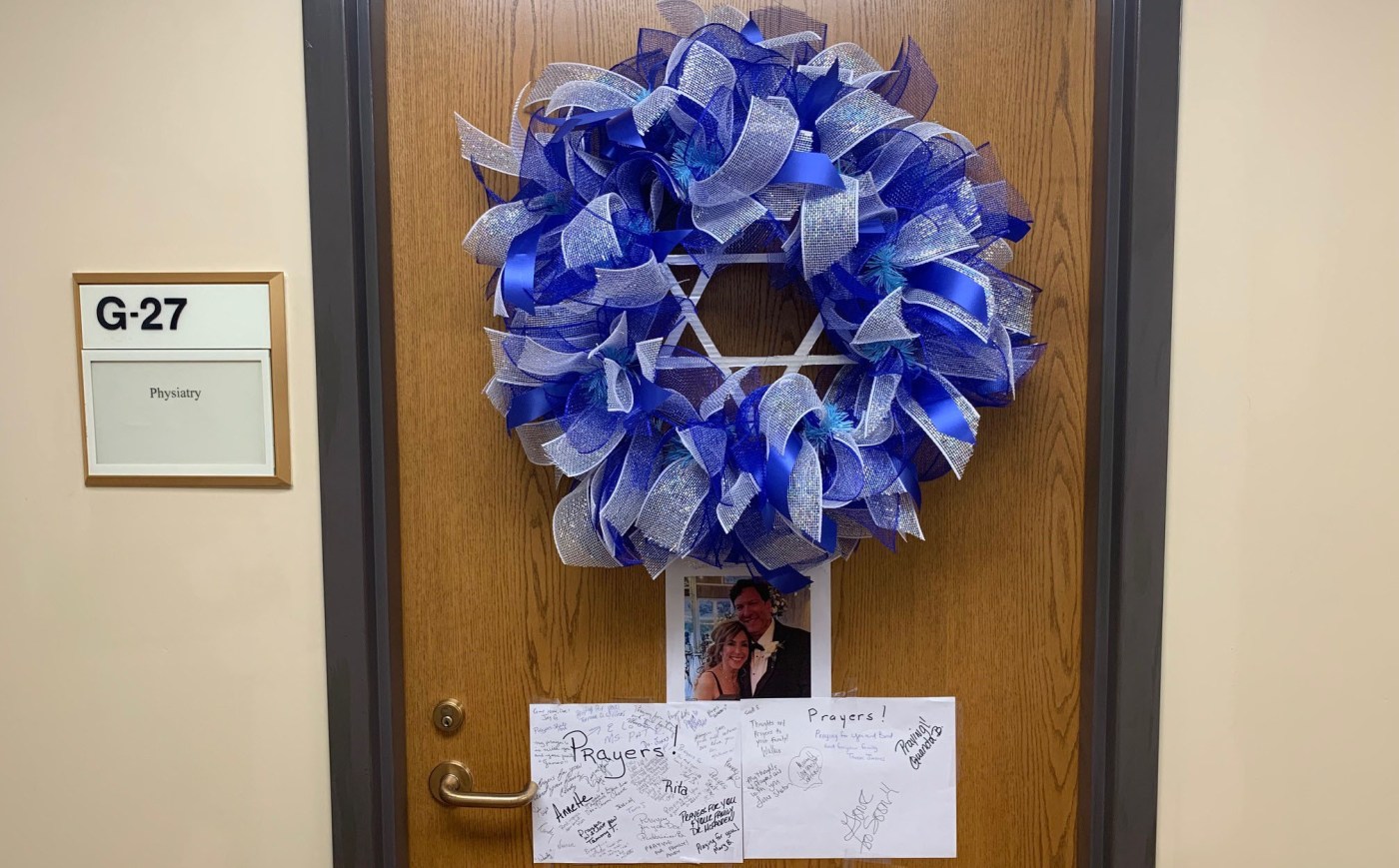
Dr. Cohen left his mark on the specialty care clinic staff and on the Tuscaloosa VA Medical Center as a whole.






sleep is very important, it is as important as food. humans need the right sleeping time.
I have PTSD and TBI injuries…my sleep is way off! I have trouble going to sleep and wake up at all times of the night. I need to try and retrain myself to sleep better